Authors: John Malaty, Lisa Gilbert, Steven Fox, Priscilla Tu, Elizabeth Close, David Voran
Introduction
When billing/coding procedures, it’s important to bill for both the procedure and the E/M visit, if applicable, using -25 modifier.
● Use the E/M code if supplementary, separately identifiable, services are provided in addition to the procedure at the same visit.
● Examples:
a. At the same visit you do a joint injection, you evaluate the etiology of a patient’s pain or other problem, i.e., diabetes mellitus or anticoagulation (with its indication) to determine safety of injection as a treatment option.
b. At the same visit you insert a long-acting contraceptive device, you perform contraceptive counseling about different options to decide on the device, discuss metrorrhagia treatment options, etc.
c. At the same visit you evaluate a patients’ pain, you do OMT.
● If a medication or drug delivery device is reimbursable, you also need to bill for it (J code). This is billed in addition to the procedure (CPT code).
● Some insurance payers require prior authorization/pre-approval before doing procedures. Ensure that this is done when needed (check with your clinic staff).
Modifier -51 (Multiple Procedures): This is used when doing more than one procedure at the same visit (when not using an “add-on code” that already has specified the number of procedures done in the code description, i.e., CPT 17003, Destruction of premalignant lesions, 2-14 does not require modifier 51).
Modifier -59 (Distinct Procedure): This is to be used when doing a distinct procedure that wouldn’t be expected to be performed at the same visit you do another procedure. It shouldn't be used when another previously established modifier is appropriate. Practically, the majority of the time Modifier -59 isn't used in outpatient Family Medicine since other modifiers are typically used. Typically, Modifier -51 is more appropriate for most of what we do, but this can get confusing (“clear as mud”) and, thus, you should check with payers in your area to determine optimal use. Half the battle may be figuring out who and what to ask (see the “Outpatient Billing and Coding” modifier section for more detail).
Important: If doing more than one procedure on the same day, report the highest-valued code first. Sometimes payment is made preferentially for the first listed code, i.e., 100% payment, with lower reimbursement for subsequently listed codes, i.e., 50% payment.
Joint/Musculoskeletal Injections
Musculoskeletal therapeutic injections are a very common office procedure for Family Medicine physicians. Patients often prefer not to go to another physician for this service. The codes for injections/aspirations are differentiated by the size of the joint and whether done without or with ultrasound (US) guidance.
|
Procedure
|
CPT
(RVU)
|
Procedure
|
CPT
(RVU)
|
|
Arthrocentesis, aspiration and/or injection, major joint or bursa (e.g., shoulder, hip, knee)
|
20610
(0.79)
|
Arthrocentesis, aspiration and/or injection, major joint or bursa (e.g., shoulder, hip, knee) with US guidance, with permanent recording and reporting
|
20611
(1.1)
|
|
Arthrocentesis, aspiration and/or injection, intermediate joint or bursa (e.g., TMJ, AC joint, wrist, elbow, ankle)
|
20605
(0.68)
|
Arthrocentesis, aspiration and/or injection, intermediate joint or bursa (e.g., TMJ, AC joint, wrist, elbow, ankle) with US guidance, with permanent recording and reporting
|
20606
(1)
|
|
Arthrocentesis, aspiration and/or injection, small joint or bursa (e.g., fingers and toes)
|
20600
(0.66)
|
Arthrocentesis, aspiration and/or injection, small joint or bursa (e.g., fingers and toes) with US guidance, with permanent recording and reporting
|
20604
(0.89)
|
Adding ultrasound guidance to improve your accuracy also adds a reasonable financial addition (RVUs and reimbursement) to the procedure. CPT requirements for US guidance include a saved US image as a permanent recording.
Procedure Modifiers:
For bilateral injections, a -50 modifier should be applied to show that the procedure was done on bilateral areas.
When doing different (or additional) injections on the same day, i.e., a knee and shoulder corticosteroid injection, a -51 modifier should be used (“multiple procedures”).
Aspiration of ganglion cyst: CPT code 20612 (RVU: 0.7)
Carpal tunnel injection: CPT 20526. (RVU: 0.94)
Trigger point injection:
● CPT 20552 - up to two muscles (RVU: 0.66)
● CPT 20553 - three or more muscles (RVU: 0.75)
● Dry needling isn’t usually covered but may change as evidence and standard of care evolves.
Tendon sheath injection, i.e., trigger finger or tenosynovitis:
● CPT 20550 - if done over tendon sheath (RVU: 0.75)
● CPT 20551 - if done at origin/insertion (RVU: 0.75)
Medication Billing: In addition to billing the CPT code for the procedure, the HCPCS code for the medication (excluding lidocaine) should be billed, i.e., J3301 for every 10mg of triamcinolone injected or J1100 for every 1mg of dexamethasone injected.
All these procedures should have documentation of medical necessity, such as pain, limitation of range of motion, impairment of activity, and what else has been tried (e.g., NSAIDs, rest, ice, physical therapy).
Women’s Health Procedures
Long Acting Reversible Contraceptives (LARCs) are very effective options for your patients, but can be very expensive to your practice if billed incorrectly (they are a high cost item). You will need to get an idea of volume to know if “buy-and-bill” or stocking a set amount is more cost effective for your practice. Some insurances require prior authorization/pre-approval before placement. You should check with your local healthcare payers. If an insurance company in your area doesn't require prior authorization, this can make it easier to do insertion the same day as a contraception discussion.
Nexplanon requires training prior to ordering/inserting. You may want to pursue training for devices you are less familiar with prior to offering them. Contacts for LARC training can be found here: https://www.acog.org/programs/long-acting-reversible-contraception-larc
Procedure Modifiers:
The -22 modifier is used for a difficult insertion, if the work is substantially more difficult than usual. Documentation must support the nature of the difficulty, the reasons for it, and the time spent vs. typical time.
The -53 modifier is used for a discontinued procedure. This provides partial payment since time was spent regardless of the outcome. It’s important to note the time spent prior to discontinuing the procedure.
The -51 modifier indicates multiple procedures were performed and is used when an IUD is removed and a new one is reinserted on the same day. Nexplanon, however, uses the single code CPT 11983 (implant reinsertion) to cover removal and reinsertion.
Note: In certain situations, ultrasound confirmation of position after placement is required following a difficult or atypically painful insertion. The ultrasound is not bundled in the IUD insertion and would be coded separately as CPT 76857 (limited non-OB pelvic US with image documentation) or CPT 76830 (trans-vaginal non-OB US with image documentation). This shouldn’t be routinely done (and billed), since it’s not standard of care/medically necessary.
Detailed coding examples can be found here: https://www.acog.org/education-and-events/publications/larc-quick-coding-guide
ICD-10 Diagnosis Codes
● Z30.014 Encounter for initial prescription of intrauterine contraceptive device (excludes insertion)
● Z30.430 Encounter for insertion of intrauterine contraceptive device
● Z30.432 Encounter for removal of intrauterine contraceptive device
● Z30.431 Encounter for routine checking of intrauterine contraceptive device (surveillance)
● Z30.433 Encounter for removal and reinsertion of intrauterine contraceptive device
● Z32.02 Pregnancy test/exam – negative
|
Category
|
CPT Code
|
Description
|
RVU
|
|
Contraception
|
11981
|
Nexplanon Insertion
|
1.48
|
|
|
11982
|
Nexplanon Removal
|
1.78
|
|
|
11983
|
Nexplanon Removal and Reinsertion
|
3.30
|
|
|
58300
|
IUD Insertion
|
1.01
|
|
|
58301
|
IUD Removal
|
1.27
|
|
Colposcopy
|
56820
|
Colpo of the vulva
|
1.5
|
|
|
56821
|
Colpo of the vulva w/biopsy
|
2.05
|
|
|
57420
|
Colpo of entire vagina w/cervix if present
|
1.6
|
|
|
57421
|
Colpo w/biopsy of vagina/cervix
|
2.20
|
|
|
57452
|
Colpo of cervix incl. upper/adj vagina
|
1.5
|
|
|
57454
|
Colpo w/bx of cervix and endo curettage
|
2.33
|
|
|
57455
|
Colpo w/bx of cervix
|
1.99
|
|
|
57456
|
Colpo w/endocervical curettage
|
1.85
|
|
|
57460
|
Colpo w/LEEP Bx of the cervix
|
2.83
|
|
|
57461
|
Colpo w/LEEP Conization of cervix
|
3.43
|
|
Endometrial Bx
|
58110
|
Endometrial Bx w/ Colp
|
0.77
|
|
|
58100
|
Endometrial Bx alone
|
1.21
|
|
Abscess
|
56405
|
I&D of vulva or perineal abscess
|
1.49
|
|
|
56420
|
I&D of Bartholin’s gland abscess
|
1.44
|
|
|
56440
|
Marsupialization of Bartholin’s gland abscess
|
2.89
|
Men’s Health and Pediatric Outpatient Procedures
|
Category
|
CPT Code
|
Description
|
RVU
|
|
Vasectomy
|
55250
|
Vasectomy
|
3.37
|
|
Circumcision
|
54150
|
Circ, using clamp or other device, newborn
|
1.9
|
|
Frenectomy
|
41115
|
Excision of lingual frenum
|
1.79
|
Dermatologic Procedures
Since malignant excisions are reimbursed at a higher rate than benign excisions, it can be helpful to hold billing or check on and edit billing after pathology returns for suspicious skin lesions. Common outpatient dermatologic procedures are listed below:
|
Category
|
CPT
Code
|
Description
|
RVU
|
|
Lesion Destruction: Premalignant & Benign Lesions, Skin, i.e., cryotherapy, curette, electro-surgery, laser, chemical treatment
|
17000
|
Destruction of premalignant lesion, 1st lesion
Premalignant, i.e., actinic keratoses
|
0.61
|
|
|
17003
|
Destruction of premalignant lesions, 2-14. Coded for each lesion (2-14).
|
0.04
|
|
|
17004
|
Destruction of >15 premalignant lesions
|
1.37
|
|
|
17110
|
Destruction of benign lesions (other than skin tags & cutaneous vascular lesions), up to 14 lesions
Benign lesions, i.e., seborrheic keratoses and warts
|
0.7
|
|
|
17111
|
Destruction of benign lesions (other than skin tags & cutaneous vascular lesions), >15
|
0.97
|
|
Skin Tag Removal
|
11200
|
Skin Tag removal, <15 skin tags
|
0.82
|
|
|
11201
|
Skin Tag removal, each additional 10 skin tags (add-on code)
|
0.29
|
|
Punch Biopsy
|
11104
|
Punch Biopsy skin, single lesion (includes simple closure when performed)
|
0.83
|
|
|
11105
|
Punch Biopsy skin, each separate/additional lesion
|
0.45
|
|
Shave biopsy/shave excision (size=lesion diameter)
|
11300
|
Trunk, Arm, Leg: <0.5 cm
|
0.6
|
|
|
11301
|
Trunk, Arm, Leg: 0.6-1.0 cm
|
0.9
|
|
|
11302
|
Trunk, Arm, Leg: 1.1-2.0 cm
|
1.05
|
|
|
11303
|
Trunk, Arm, Leg: >2.0 cm
|
1.25
|
|
|
11305
|
Scalp, Neck, Hands, Feet, Genital: <0.5 cm
|
0.8
|
|
|
11306
|
Scalp, Neck, Hands, Feet, Genital: 0.6-1.0 cm
|
0.96
|
|
|
11307
|
Scalp, Neck, Hands, Feet, Genital: 1.1-2.0 cm
|
1.2
|
|
|
11308
|
Scalp, Neck, Hands, Feet, Genital: >2.0 cm
|
1.46
|
|
|
11310
|
Face, Ears, Eyelids, Lids, Nose, Lips, Mucous Membrane: <0.5 cm
|
0.8
|
|
|
11311
|
Face, Ears, Eyelids, Lids, Nose, Lips, Mucous Membrane: 0.6-1.0 cm
|
1.1
|
|
|
11312
|
Face, Ears, Eyelids, Lids, Nose, Lips, Mucous Membrane: 1.1-2.0 cm
|
1.3
|
|
|
11313
|
Face, Ears, Eyelids, Lids, Nose, Lips, Mucous Membrane: >2.0 cm
|
1.68
|
|
Benign excision, i.e., wide local excision (size=excised diameter, includes lesion + margins)
|
11400
|
Trunk, Arm, Leg: <0.5 cm
|
0.9
|
|
|
11401
|
Trunk, Arm, Leg: 0.6-1.0 cm
|
1.28
|
|
|
11402
|
Trunk, Arm, Leg: 1.1-2.0 cm
|
1.45
|
|
|
11403
|
Trunk, Arm, Leg: 2.1-3 cm
|
1.84
|
|
|
11404
|
Trunk, Arm, Leg: 3.1-4 cm
|
2.11
|
|
|
11406
|
Trunk, Arm, Leg: >4 cm
|
3.52
|
|
|
11420
|
Scalp, Neck, Hands, Feet, Genital: <0.5 cm
|
1.03
|
|
|
11421
|
Scalp, Neck, Hands, Feet, Genital: 0.6-1.0 cm
|
1.47
|
|
|
11422
|
Scalp, Neck, Hands, Feet, Genital: 1.1-2.0 cm
|
1.68
|
|
|
11423
|
Scalp, Neck, Hands, Feet, Genital: 2.1-3 cm
|
2.06
|
|
|
11424
|
Scalp, Neck, Hands, Feet, Genital: 3.1-4 cm
|
2.48
|
|
|
11426
|
Scalp, Neck, Hands, Feet, Genital: >4 cm
|
4.09
|
|
|
11440
|
Face, Ears, Eyelids, Lids, Nose, Lips, Mucous Membrane: <0.5 cm
|
1.05
|
|
|
11441
|
Face, Ears, Eyelids, Lids, Nose, Lips, Mucous Membrane: 0.6-1.0 cm
|
1.53
|
|
|
11442
|
Face, Ears, Eyelids, Lids, Nose, Lips, Mucous Membrane: 1.1-2.0 cm
|
1.77
|
|
|
11443
|
Face, Ears, Eyelids, Lids, Nose, Lips, Mucous Membrane: 2.1-3.0 cm
|
2.34
|
|
|
11444
|
Face, Ears, Eyelids, Lids, Nose, Lips, Mucous Membrane: 3.1-4.0 cm
|
3.19
|
|
|
11446
|
Face, Ears, Eyelids, Lids, Nose, Lips, Mucous Membrane: >4.0 cm
|
4.80
|
|
Malignant Excision, i.e., wide local excision (size=excised diameter, includes lesion + margins)
|
11600
|
Trunk, Arm, Leg: <0.5 cm
|
1.63
|
|
|
11601
|
Trunk, Arm, Leg: 0.6-1.0 cm
|
2.07
|
|
|
11602
|
Trunk, Arm, Leg: 1.1-2.0 cm
|
2.27
|
|
|
11603
|
Trunk, Arm, Leg: 2.1-3 cm
|
2.82
|
|
|
11604
|
Trunk, Arm, Leg: 3.1-4 cm
|
3.17
|
|
|
11606
|
Trunk, Arm, Leg: >4 cm
|
5.02
|
|
|
11620
|
Scalp, Neck, Hands, Feet, Genital: <0.5 cm
|
1.64
|
|
|
11621
|
Scalp, Neck, Hands, Feet, Genital: 0.6-1.0 cm
|
2.08
|
|
|
11622
|
Scalp, Neck, Hands, Feet, Genital: 1.1-2.0 cm
|
2.41
|
|
|
11623
|
Scalp, Neck, Hands, Feet, Genital: 2.1-3 cm
|
3.11
|
|
|
11624
|
Scalp, Neck, Hands, Feet, Genital: 3.1-4 cm
|
3.62
|
|
|
11626
|
Scalp, Neck, Hands, Feet, Genital: >4 cm
|
4.61
|
|
|
11640
|
Face, Ears, Eyelids, Lids, Nose, Lips: <0.5 cm
|
1.67
|
|
|
11641
|
Face, Ears, Eyelids, Lids, Nose, Lips: 0.6-1.0 cm
|
2.17
|
|
|
11642
|
Face, Ears, Eyelids, Lids, Nose, Lips: 1.1-2.0 cm
|
2.62
|
|
|
11643
|
Face, Ears, Eyelids, Lids, Nose, Lips: 2.1-3.0 cm
|
3.42
|
|
|
11644
|
Face, Ears, Eyelids, Lids, Nose, Lips: 3.1-4.0 cm
|
4.34
|
|
|
11646
|
Face, Ears, Eyelids, Lids, Nose, Lips: >4.0 cm
|
6.26
|
|
Malignant Destruction, Skin,
i.e., cryotherapy, curette, electrosurgery, laser, chemical treatment
|
17260
|
Trunk, Arm, Leg: <0.5 cm
|
0.96
|
|
|
17261
|
Trunk, Arm, Leg: 0.6-1.0 cm
|
1.22
|
|
|
17262
|
Trunk, Arm, Leg: 1.1-2.0 cm
|
1.63
|
|
|
17263
|
Trunk, Arm, Leg: 2.1-3.0 cm
|
1.84
|
|
|
17264
|
Trunk, Arm, Leg: 3.1-4.0 cm
|
1.99
|
|
|
17266
|
Trunk, Arm, Leg: >4.0 cm
|
2.39
|
|
|
17270
|
Scalp, Neck, Hands, Feet, Genital: <0.5 cm
|
1.37
|
|
|
17271
|
Scalp, Neck, Hands, Feet, Genital: 0.6-1.0 cm
|
1.54
|
|
|
17272
|
Scalp, Neck, Hands, Feet, Genital: 1.1-2.0 cm
|
1.82
|
|
|
17273
|
Scalp, Neck, Hands, Feet, Genital 2.1-3.0 cm
|
2.1
|
|
|
17274
|
Scalp, Neck, Hands, Feet, Genital: 3.1-4.0 cm
|
2.64
|
|
|
17276
|
Scalp, Neck, Hands, Feet, Genital: >4.0 cm
|
3.25
|
|
|
17280
|
Face, Ears, Eyelids, Nose, Lips, Mucous Membrane: <0.5 cm
|
1.22
|
|
|
17281
|
Face, Ears, Eyelids, Nose, Lips, Mucous Membrane: 0.6-1.0 cm
|
1.77
|
|
|
17282
|
Face, Ears, Eyelids, Nose, Lips, Mucous Membrane: 1.1-2.0 cm
|
2.09
|
|
|
17283
|
Face, Ears, Eyelids, Nose, Lips, Mucous Membrane: 2.1-3.0 cm
|
2.69
|
|
|
17284
|
Face, Ears, Eyelids, Nose, Lips, Mucous Membrane: 3.1-4.0 cm
|
3.2
|
|
|
17286
|
Face, Ears, Eyelids, Nose, Lips, Mucous Membrane: >4.0 cm
|
4.48
|
|
Incision and Drainage
|
10060
|
Drain Skin Abscess, simple/single
|
1.22
|
|
|
10061
|
Drain Skin Abscess, complex/multiple
|
2.45
|
|
|
10080
|
I&D Pilonidal Cyst, simple
|
1.22
|
|
|
10081
|
I&D Pilonidal Cyst, complicated
|
2.5
|
|
|
10140
|
I&D hematoma, seroma, or fluid collect
|
1.58
|
|
|
10180
|
I&D, complex, postoperative wound infection
|
2.3
|
|
Incision & Removal Foreign Body
|
10120
|
I&R foreign body, subcutaneous, simple
|
1.22
|
|
|
10121
|
I&R foreign body, subcutaneous, complicated
|
2.74
|
|
Simple Laceration or wound repair (1 layer closure)
|
12001
|
Scalp, Neck, Axilla, Genitalia, Trunk, Extremity: 2.5 cm or less
|
0.84
|
|
|
12002
|
Scalp, Neck, Axilla, Genitalia, Trunk, Extremity: 2.6-7.5 cm
|
1.14
|
|
|
12004
|
Scalp, Neck, Axilla, Genitalia, Trunk, Extremity: 7.6-12.5 cm
|
1.44
|
|
|
12005
|
Scalp, Neck, Axilla, Genitalia, Trunk, Extremity: 12.6-20.0 cm
|
1.97
|
|
|
12006
|
Scalp, Neck, Axilla, Genitalia, Trunk, Extremity: 20.1-30.0 cm
|
2.39
|
|
|
12007
|
Scalp, Neck, Axilla, Genitalia, Trunk, Extremity: >30 cm
|
2.9
|
|
|
12011
|
Face, Ears, Eyelids, Nose, Lips, Mucous Membrane: 2.5 cm or less
|
1.07
|
|
|
12013
|
Face, Ears, Eyelids, Nose, Lips, Mucous Membrane: 2.6-5.0 cm
|
1.22
|
|
|
12014
|
Face, Ears, Eyelids, Nose, Lips, Mucous Membrane: 5.1-7.5 cm
|
1.57
|
|
|
12015
|
Face, Ears, Eyelids, Nose, Lips, Mucous Membrane: 7.6-12.5 cm
|
1.98
|
|
|
12016
|
Face, Ears, Eyelids, Nose, Lips, Mucous Membrane: 12.6-20.0 cm
|
2.68
|
|
|
12017
|
Face, Ears, Eyelids, Nose, Lips, Mucous Membrane: 20.1-30.0 cm
|
3.18
|
|
|
12018
|
Face, Ears, Eyelids, Nose, Lips, Mucous Membrane: >30.0 cm
|
3.61
|
|
Intermediate Laceration or wound repair (requires layered closure of skin, including one or more subcutaneous or non-muscle fascial areas)
|
12017
|
Scalp, Axilla, Trunk, Arm, or Leg: 2.5cm or less
|
2
|
|
|
12032
|
Scalp, Axilla, Trunk, Arm, or Leg: 2.6-7.5 cm
|
2.52
|
|
|
12034
|
Scalp, Axilla, Trunk, Arm, or Leg: 7.6-12.5 cm
|
2.97
|
|
|
12035
|
Scalp, Axilla, Trunk, Arm, or Leg: 12.6-20.0 cm
|
3.50
|
|
|
12036
|
Scalp, Axilla, Trunk, Arm, or Leg: 20.1-30.0 cm
|
4.23
|
|
|
12037
|
Scalp, Axilla, Trunk, Arm, or Leg: >30 cm
|
5
|
|
|
12041
|
Neck, Hand, Foot, Genitalia: 2.5 cm or less
|
2.1
|
|
|
12042
|
Neck, Hand, Foot, Genitalia: 2.6-7.5 cm
|
2.79
|
|
|
12044
|
Neck, Hand, Foot, Genitalia: 7.6-12.5 cm
|
3.19
|
|
|
12045
|
Neck, Hand, Foot, Genitalia: 12.6-20.0 cm
|
3.75
|
|
|
12046
|
Neck, Hand, Foot, Genitalia: 20.1-30.0 cm
|
4.30
|
|
|
12047
|
Neck, Hand, Foot, Genitalia: >30 cm
|
4.95
|
|
|
12051
|
Face, Ears, Eyelids, Nose, Lips, Mucous Membrane: 2.5 cm or less
|
2.33
|
|
|
12052
|
Face, Ears, Eyelids, Nose, Lips, Mucous Membrane: 2.6-5.0 cm
|
2.87
|
|
|
12053
|
Face, Ears, Eyelids, Nose, Lips, Mucous Membrane: 5.1-7.5 cm
|
3.17
|
|
|
12054
|
Face, Ears, Eyelids, Nose, Lips, Mucous Membrane: 7.6-12.5 cm
|
3.50
|
|
|
12055
|
Face, Ears, Eyelids, Nose, Lips, Mucous Membrane: 12.6-20.0 cm
|
4.50
|
|
|
12056
|
Face, Ears, Eyelids, Nose, Lips, Mucous Membrane: 20.1-30.0 cm
|
5.30
|
|
|
12057
|
Face, Ears, Eyelids, Nose, Lips, Mucous Membrane: >30.0 cm
|
6.00
|
|
Complex Laceration/Wound Repair (must be >1.1cm; may include scar revision, extensive under-mining, debridement, or retention suture replacement).
|
13100
|
Trunk: 1.1-2.5 cm
|
3.00
|
|
|
13101
|
Trunk: 2.6-7.5 cm
|
3.50
|
|
|
13102
|
Trunk add-on code: each additional 5 cm
|
1.24
|
|
|
13120
|
Scalp, Arm, or Leg: 1.1-2.5 cm
|
3.23
|
|
|
13121
|
Scalp, Arm, or Leg: 2.6-7.5 cm
|
4.00
|
|
|
13122
|
Scalp, Arm, or Leg add-on code: each add’l 5 cm
|
1.44
|
|
|
13131
|
Forehead, Cheek, Chin, Mouth, Neck, Axilla, Genitalia, Hand, or Foot: 1.1-2.5 cm
|
3.73
|
|
|
13132
|
Forehead, Cheek, Chin, Mouth, Neck, Axilla, Genitalia, Hand, or Foot: 2.6-7.5 cm
|
4.78
|
|
|
13133
|
Forehead, Cheek, Chin, Mouth, Neck, Axilla, Genitalia, Hand, or Foot add-on code: each additional 5 cm
|
2.19
|
|
|
13151
|
Ear, Nose, Eyelid, or Lip: 1.1-2.5 cm
|
4.34
|
|
|
13152
|
Ear, Nose, Eyelid, or Lip: 2.6-7.5 cm
|
5.34
|
|
|
13153
|
Ear, Nose, Eyelid, or Lip add on code: each additional 5 cm
|
2.38
|
|
Wound Care
|
11042
|
Debridement, subcutaneous tissue (includes epidermis and dermis, if performed); first 20 square cm or less
|
1.01
|
|
|
11045
|
Add-on code for 11042: each additional 20 square cm, or part thereof
|
0.5
|
|
|
11043
|
Debridement, muscle and/or fascia (includes epidermis, dermis and subcutaneous tissue, if performed); first 20 square cm or less
|
2.7
|
|
|
11046
|
Add-on code for 11043: each additional 20 square cm, or part thereof
|
1.03
|
|
Nail Care
|
11719
|
Trimming, nondystrophic nail(s), any number
|
0.17
|
|
|
G0127
|
Trimming dystrophic nail(s), any number
|
0.17
|
|
|
11720
|
Debridement: up to 5 nails
|
0.32
|
|
|
11721
|
Debridement: >6 nails
|
0.54
|
|
|
11730
|
Avulsion of nail plate
|
1.05
|
|
|
11732
|
Avulsion add-on code: each additional nail plate
|
0.38
|
|
|
11750
|
Excision of Nail Matrix, Permanent Removal
|
1.58
|
|
|
11755
|
Nail biopsy
|
1.25
|
Osteopathic Manipulative Procedures (OMT)
Osteopathic manipulative treatment (OMT) is a procedure used primarily by osteopathic physicians to treat qualifying somatic dysfunctions, defined as the “impaired or altered function of related components of the somatic (body framework) system.”1 Reimbursement for the procedure began in 1974 with the work of Dr. Edward Stiles, and continues today through appropriate documentation and billing of the evaluation and procedure.2
Multiple aspects of treatment impact documenting and billing for an OMT visit. It's necessary to manage each part correctly to avoid denial of the claim. Sometimes, even with appropriate documentation and billing, claims are denied. Therefore, having a solid understanding of all aspects of the treatment, as well as common misconceptions about it, can aid in appealing those claims and increase awareness and appreciation of OMT.3
Evaluation and Management (E&M)
Most encounters are coded based on the evaluation and management of the presenting problem. Documentation must include medical decision-making, with supportive history and physical exam, even if a patient was seen previously and had OMT performed. Thus, each encounter typically includes discussion of the patient’s symptoms from the last procedure until the time of the current visit. It is helpful to include exam details of inspection for asymmetry, palpation, tenderness, range of motion, muscle strength and tone, and any somatic dysfunctions found.4 Appropriate and universal documentation should be used for documenting somatic dysfunctions (i.e., named for the direction of ease and in all planes of motion). Commonly understood shorthand may be used. For example, a dysfunction of the seventh thoracic vertebral segment (T7) in flexion (F), left side bending (sL) and left rotation (rL) can be documented as T7 FsLrL.
Most E&M codes for OMT will be in the outpatient setting as new (99202-99205) or established (99211-99215) patients, with -25 modifier (see outpatient coding section for more detail). However, OMT can be used within an Emergency Department visit,6 on the inpatient service,7 or as a consult visit (99241-99245). Consultant codes can often be declined, however, if an appropriate referral was made and the family-medicine specialist is able to offer opinion and treatment to the referring provider who isn’t trained to do OMT, consultative billing may apply.2
ICD-10 Codes
While ICD-10 codes for somatic dysfunctions (M99.00-M99.09) must be noted for the OMT procedure, they should be accompanied by the diagnosis codes for the condition as well. For example, a patient with low back pain and somatic dysfunctions noted in the lumbar, thoracic, pelvis, and sacral regions should have five diagnoses: low back pain (M54.5) and somatic dysfunctions of the noted segments (M99.03, M99.02, M99.05, and M99.04, respectively). The low back pain diagnosis should be associated with the E&M service code, while the somatic dysfunctions are associated with the OMT CPT code. See Table 1 for ICD-10 codes for OMT:
Table 1 – ICD-10 Codes for OMT
|
ICD-10 Code
|
Description of Code
|
|
M99.00
|
Segmental and somatic dysfunction of head region
|
|
M99.01
|
Segmental and somatic dysfunction of cervical region
|
|
M99.02
|
Segmental and somatic dysfunction of thoracic region
|
|
M99.03
|
Segmental and somatic dysfunction of lumbar region
|
|
M99.04
|
Segmental and somatic dysfunction of sacral region
|
|
M99.05
|
Segmental and somatic dysfunction of pelvic region
|
|
M99.06
|
Segmental and somatic dysfunction of lower extremity
|
|
M99.07
|
Segmental and somatic dysfunction of upper extremity
|
|
M99.08
|
Segmental and somatic dysfunction of rib cage
|
|
M99.09
|
Segmental and somatic dysfunction of abdomen and other regions
|
Current Procedural Terminology (CPT) Codes
Billing for the OMT procedure is fairly straightforward and dependent on the number of regions treated. The above ICD-10 codes are associated with the OMT CPT Codes (Table 2). These codes are specific to OMT performed by physicians and shouldn’t be confused with manipulation codes done by physical therapists, chiropractors, or massage therapists, which often have annual limitations placed on them.
Table 2 – CPT Codes for OMT
|
CPT Code
|
Description of Code
|
RVU
|
|
98925
|
Osteopathic manipulative treatment to 1 or 2 body regions
|
0.46
|
|
98926
|
Osteopathic manipulative treatment to 3 or 4 body regions
|
0.71
|
|
98927
|
Osteopathic manipulative treatment to 5 or 6 body regions
|
0.96
|
|
98928
|
Osteopathic manipulative treatment to 7 or 8 body regions
|
1.21
|
|
98929
|
Osteopathic manipulative treatment to 9 or 10 body regions
|
1.46
|
Bundling
A common denial from payers is not reimbursing the E&M for the encounter but, instead, bundling it in with the OMT CPT code. Good documentation is important. Part of the decision-making includes whether or not to utilize OMT as a treatment option, and this decision must be made at each encounter. If the decision is made to utilize OMT, then procedure is performed and documented. Often, it’s helpful to have separate notes for the procedure and for the E&M.12
Case Examples:
1. New patient with low back pain
CC: Low back pain
S: SLB is a 36-year-old Caucasian male new patient complaining of low back pain for 3 days after helping a friend move. He describes pain with changes of position and has used ibuprofen and ice with some relief. He denies paresthesia, incontinence, radiation of pain, numbness or tingling. He has no significant medical or surgical history. Other than ibuprofen, he uses a fluticasone nasal spray daily and has no drug allergies. ROS otherwise negative.
O: Vitals are normal. He is slightly flexed at the lumbar spine with muscle spasms and tenderness to palpation of the lumbar region paraspinal muscles. There is mild decreased active range of motion of spine in flexion and extension due to pain but full passive. Neurological and muscle strength testing are normal. Osteopathic exam: T10-L4 NrLsR; L5 FrRsR; R innominate posterior; L on L sacral rotation.
A: 1. Lumbar muscle strain (S39.012A) 2. Somatic dysfunction of thoracic, lumbar, sacrum, pelvis (M99.02, M99.03, M99.04, M99.05).
P: 1. OMT was discussed and performed during this visit (see Procedure Note below). 2. Continue ibuprofen and ice to area as needed. 3. Flexeril prescribed at bedtime. 4. Drink plenty of water today and tomorrow. 5. Return in 1 week for follow up.
Procedure Note: Risks and benefits of OMT discussed with patient who elected for procedure. OMT techniques utilizing soft tissue, muscle energy, and facilitated positional release performed with improvement of dysfunction and pain. Patient tolerated procedure well and was given post-procedure instructions.
Billing: 99203 E&M (New patient, level 3) associated with S39.012A, Modifier-25, 98926 (OMT 4 regions) associated with somatic dysfunction diagnoses.
2. Established Patient – Follow up above patient
CC: Low back pain
S: SLB is a 36-year-old Caucasian male patient here for follow up of low back pain. After his last visit, he has been able to move better with decreased pain. He still feels stiff occasionally and continues to use ibuprofen and ice, but with decreasing frequency. He continues to deny radiation, numbness, tingling, and radiation. There are no changes to his medications, allergies, or medical history. Remainder of ROS negative.
O: Vitals are normal. He has normal posture with mild hypertonicity and tenderness to palpation of the lumbar region paraspinal muscles. Active range of motion of spine is full with some pain in extension of lumbar spine. Neurological and muscle strength testing are normal. Osteopathic exam: L5 FrRsR; R sacral extension.
A: 1. Lumbar muscle strain improving (S39.012A) 2. Somatic dysfunction of lumbar, sacrum improving (M99.03, M99.04).
P: 1. OMT was discussed and performed this visit (see below procedure note). 2. Continue ibuprofen and ice to area as needed. 3. Drink plenty of water today and tomorrow. 4. Gentle stretching demonstrated and encouraged. 5. Instructed on proper technique with lifting heavy objects. 6. Return as needed or if no continued improvement.
Procedure Note: Risks and benefits of OMT discussed with patient who elected for procedure. OMT techniques utilizing soft tissue, muscle energy, and facilitated positional release performed with improvement of dysfunction and pain. Patient tolerated procedure well and given post-procedure instructions.
Billing: 99213 E&M (Established patient level 3) associated with S39.012A, Modifier-25, 98925 (OMT 2 regions) associated with somatic dysfunction diagnoses.
References for OMT Billing
- Ward RC, ed. Foundations for Osteopathic Medicine. 2nd ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2003: 1240,1249.
- Jorgensen DJ. OMT coding strategies to boost your bottom line: Implement these strategies for better OMT reimbursement. https://www.acofp.org/ACOFPIMIS/Acofporg/Practice_Management/OMT_Coding_Strategies.aspx?WebsiteKey=fc4f41d1-af75-443c-a928-3d7d67bac6a7. Accessed December 27, 2019.
- https://www.acgme.org/What-We-Do/Recognition/Osteopathic-Recognition. Accessed December 27, 2019
- Snider KT, Jorgensen DJ. Billing and coding for osteopathic manipulative treatment. J Am Osteopath Assoc. 2009 Aug;109(8):409-13
- 5. https://www.academyofosteopathy.org/practice-management. Accessed December 27, 2019.
- Ault B, Levy D. Osteopathic manipulative treatment use in the emergency department: A retrospective medical record review. J Am Osteopath Assoc 2015 Mar; 115(3): 132-7.
- Snider KT, Snider EJ, DeGooyer BR, Bukowski AM, Fleming RK, Johnson JC. Retrospective medical record review of an osteopathic manipulative medicine hospital consultation service. J Am Osteopath Assoc. 2013 Oct;113(10):754-67.
- Felger TA, Felger M. Getting paid: Understanding when to use modifier-25. Fam Pract Manag 2004 Oct; 11(9):21.22.
- https://www.cms.gov/Medicare/Coding/NationalCorrectCodInitEd/downloads/modifier59.pdf. Accessed December 27, 2019.
- 0 https://www.aafp.org/journals/fpm/blogs/gettingpaid/entry/medicare_plans_new_coding_modifiers.html?_ga=2.184775017.1795524355.1577404332-631379629.1547927235. Accessed December 27, 2019.
- 1. https://osteopathic.org/practicing-medicine/business-of-medicine/osteopathic-billing-coding/. Accessed December 27, 2019.
Spirometry
 Spirometry is a method of assessing lung function by measuring the volume and velocity of air expelled from the lungs after maximal inspiration. Spirometry is a simple procedure, can easily be performed in an office setting, and is often reimbursed as much as the entire office visit. Unfortunately, it's one of the most overlooked procedures by family physicians. This procedure is required for the diagnosis of several pulmonary diseases, is a required quality metric for patients newly diagnosed with COPD, and enhances the revenue of the office. Following is a list of reasons for performing this procedure in the office:
Spirometry is a method of assessing lung function by measuring the volume and velocity of air expelled from the lungs after maximal inspiration. Spirometry is a simple procedure, can easily be performed in an office setting, and is often reimbursed as much as the entire office visit. Unfortunately, it's one of the most overlooked procedures by family physicians. This procedure is required for the diagnosis of several pulmonary diseases, is a required quality metric for patients newly diagnosed with COPD, and enhances the revenue of the office. Following is a list of reasons for performing this procedure in the office:
● Screen those at risk for respiratory diseases
● Differentiates between obstructive and restrictive diseases
● Evaluate respiratory symptoms
● Assess and monitor disease progression
● Assess response to therapy
● Correlate with abnormal X-rays
● Perform pre-operative assessment
● Needed for diagnosis of COPD
● Monitor for adverse reactions to drugs with known pulmonary toxicity
● Screen workforces in occupational medicine
● Assess rehab patients
● Assess fitness to dive
● Pre-employment screenings in certain professions
How often should spirometry be performed? When is it indicated? Much more often than most Family Physicians realize. Spirometry is indicated for any of the following reasons:
● Unexplained, frequent, and/or persistent dyspnea
● Unexplained, frequent and/or persistent cough
● Chronic wheezing
● Any patient with suspected COPD who has never had spirometry
● Any patient with suspected asthma who has never had spirometry
● Assessment of asthma control within 2-6 weeks after initiating treatment, and at least every 1-2 years
● Basic preoperative evaluation of lung function in patients with lung disease
● Smokers over 40 with persistent cough
● Anyone with frequent colds
● Patients with allergic rhinitis
● Occupational exposure to dust and chemicals
● Patients with deformities involving the thorax
o Scoliosis
o Pectus carinatum (pigeon chest) and excavatum
o Barrel chested patients
Rarely a day goes by that a Family Physician will not see a patient meeting one or more of these indications. However, there are some contraindications to performing this procedure in the clinic. The primary contraindication pertains to those with conditions or active diseases, or those who can’t understand or follow instructions. Some include:
● tracheostomies
● active lung disease
● hemoptysis
● respiratory distress
● nausea or vomiting
● unresolved pneumothorax
● Unstable angina or myocardial infarction in the last month
● Recent pulmonary embolism in last month
● Recent eye, ear, oral, brain or cardiothoracic surgeries in last 3 months
One of the often overlooked aspects of spirometry is the reimbursement to the clinic performing this procedure, as the following table shows:
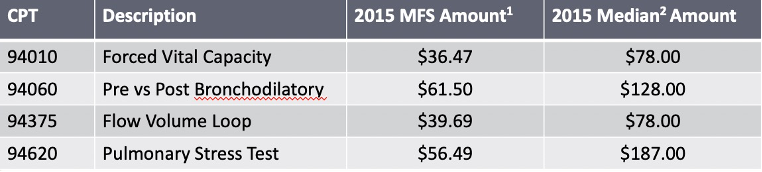
Figure 1. CPT Codes and typical spirometry procedure reimbursements
1 The global fees above represent the sum of the technical and interpretive components based on Medicare Fee Schedule amounts for 2015. Individual physician rates are affected by a geographic practice cost index factor based on practice location.
NOTE: Commercial insurer payments may differ. These figures are intended as guidelines only, and may be subject to change.
2 The median or 50th percentile of usual, customary, and reasonable (UCR) fees are reflective of payer allowables and based on analysis of health insurance claims submitted to third-party payers.
These reimbursements compare favorably with normal 9920x and 9921x CPT codes (Figure 2)[1]
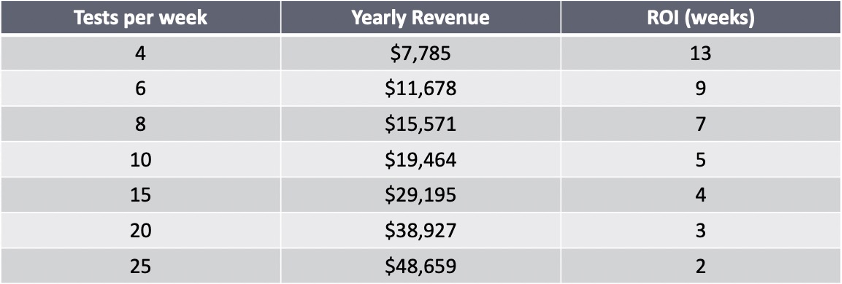
Figure 2. Projected spirometry revenue based on number of procedures per week
How expensive are spirometers? They range in price from $100 to $3,000. The less expensive ones display the results, but don’t generate an output that can be imported into EHRs. Many spirometers have printouts that can be scanned into the EHR or produce an output that can be directly interfaced with an EHR. Considering cost and revenue, the return on investment can be favorable in less than 6 months for most devices (not including the most expensive devices).
As an example of the return on investment, one residency clinic (Truman Medical Center: Lakewood’s Family Medicine Center) made a $4,000 investment for 3 Winspiro devices and 30 networked station licenses in May of 2015. A Grand Rounds presentation was given during which all 36 residents participated in training to perform this procedure. Without a great deal of further education, they performed over 600 of these in the residency clinic in 4 years since purchasing the equipment. These tests generated an estimated $61,900 in additional revenue, easily recouping initial investment in the equipment.
Incorporating this diagnostic tool into the clinic enabled this site to meet their registry measures and improve HEDIS reporting to their managed care partners.
Inpatient Procedure Codes
|
Code
|
Description
|
RVU
|
|
62270
|
Lumbar puncture - diagnostic
|
1.22
|
|
49082
|
Abdominal paracentesis
|
1.24
|
|
49083
|
US guided abdominal paracentesis
|
2
|
|
32554
|
Thoracentesis, needle or catheter, aspiration of the pleural space; without imaging guidance
|
1.82
|
|
32555
|
Thoracentesis, needle or catheter, aspiration of the pleural space; with imaging guidance
|
2.27
|
|
32556
|
Pleural drainage, percutaneous, with insertion of indwelling catheter; without imaging guidance
|
2.50
|
|
32551
|
Insertion of chest tube
|
3.04
|
|
99465
|
Newborn resuscitation
|
2.93
|
|
92950
|
Cardiopulmonary resuscitation
|
4
|
|
31500
|
Intubation, endotracheal, emergency procedure
|
3
|
|
93018
|
Inpatient: Cardiovascular stress test using maximal or submaximal treadmill or bicycle exercise, continuous electrocardiographic monitoring, and/or pharmacological stress; interpretation and report only
|
0.30
|